OUR HEALTH PRIORITIES

Our historic mission
Solthis was initially created to combat the HIV epidemic and provide broad access to high-quality, sustainable care. In 2003, epidemiological data was alarming, with mortality and incidence rates continuing to rise in Africa and access to antiretroviral treatment meeting only a tiny fraction of the need.
The fight against HIV in West and Central Africa: Challenges and priorities
In West and Central Africa, HIV remains a major public health challenge. Despite 20 years of commitment and response and a significant decline in mortality (-55%) and new infections (-46%), in 2023 the region still had approximately 5.1 million people living with HIV, with 190,000 new infections and 130,000 deaths. Although progress is encouraging – 81% of people living with HIV know their status, 77% are on treatment, and 70% have an undetectable viral load – vulnerabilities remain, which justify our continued work: Children and adolescents living with HIV are neglected: only 35% receive treatment. Prevention of mother-to-child transmission remains inadequate: 46% of pregnant women living with HIV are not treated and 20% of newborns are infected and underdiagnosed due to insufficient access to early diagnosis (26%). Adolescent girls and young women (aged 15-24) account for 19% of new infections, linked to gender inequalities, gender-based violence, and poor access to sex education. Key populations (sex workers, men who have sex with men, people who inject drugs) and their partners account for 34% of new infections. Their access to care remains limited and is hampered by stigma, criminalization (92% of countries for sex work and 48% for same-sex relations), inadequate care provision, and still very limited access to prevention (PrEP) or harm reduction programs. Other more specific challenges must be addressed to ensure the long-term success of the fight against HIV in the region. HIV diagnosis happens too late: nearly half of people found out their HIV status at an advanced stage and often have opportunistic infections, in a context of inadequate diagnostic and therapeutic resources. Stigma remains among the highest in the world, affecting access to testing, the quality of care, the care relationship, retention in treatment, and the quality of life of those affected. While the current dolutegravir-based treatment appears to be effective and well tolerated, supply disruptions threaten continuity. The identification and management of treatment failures and side effects remains very limited. Innovations, such as long-acting injectable treatments, are not yet available. Aging among people living with HIV is leading to an increase in comorbidities (diabetes, cardiovascular and renal diseases, etc.), for which care is still poorly structured and often unavailable. Finally, the almost total financial dependence of countries on international donors to respond to HIV undermines the sustainability of progress.
Leading cause of infectious mortality among people living with HIV
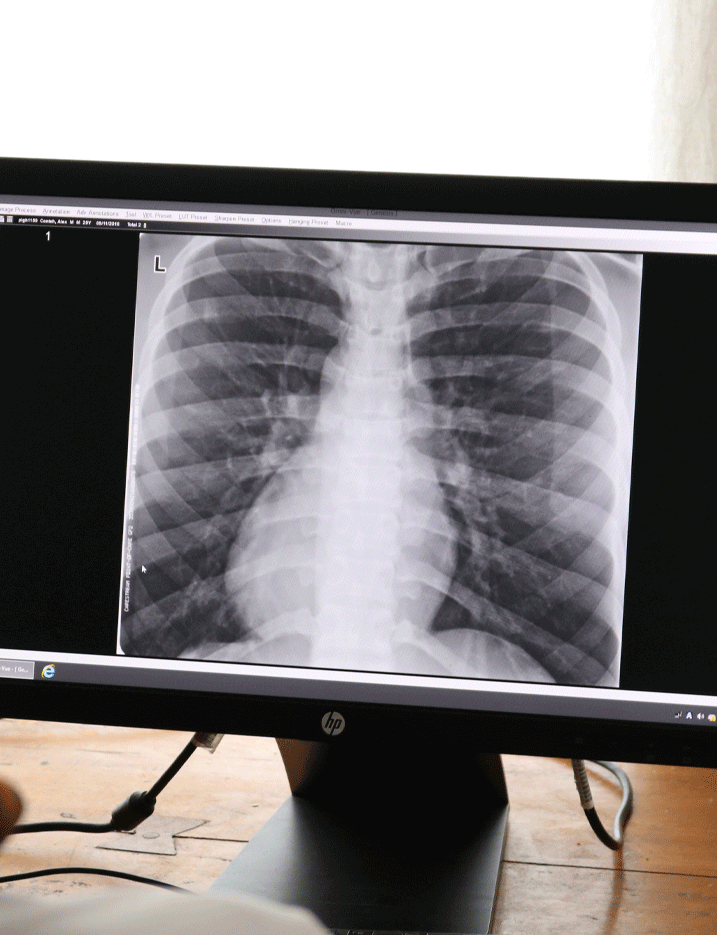
Although there has been a 27% decline in incidence and a 38% decline in mortality between 2015 and 2023 in sub-Saharan Africa, tuberculosis remains the leading cause of death from an infectious disease. In 2023, approximately 10.8 million people contracted the disease and 8.2 million people were diagnosed worldwide, while 1.25 million died, including 161,000 people living with HIV, making it the leading cause of death among this group.
Many challenges remain
In addition to challenges related to weak health systems, malnutrition, exacerbated by climate change, and volatile living conditions, aggravated by population displacement following crises and conflicts, fuel the transmission of tuberculosis.
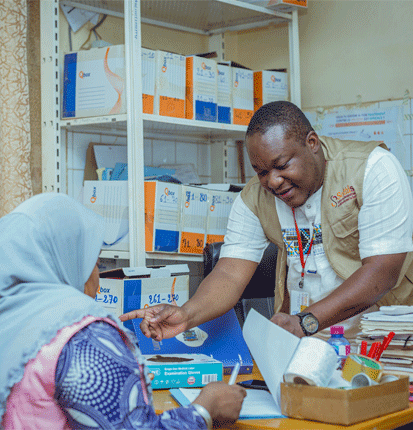
Access to screening remains a challenge. A quarter of cases still go undiagnosed, and diagnosis often happens late. Among the many reasons for this are poor access to X-rays, rapid urine tests for people living with HIV, and rapid molecular tests (48%), which limits the identification of multi-drug resistant forms of TB.
Although women are generally less affected by TB than men, the peripartum period is a time of risk, however this remains largely overlooked by public health programs. Young children are also particularly affected: it is estimated that of the 191,000 annual deaths linked to tuberculosis, 96% were not diagnosed and treated, despite the development of new diagnostic tools that are slow to be implemented. Certain populations, such as prisoners and people with chronic conditions such as diabetes, are particularly affected but are still not sufficiently identified by TB control programs.
Access to treatment and therapeutic success rates for drug-sensitive TB are satisfactory (88%), but this should not obscure the dramatic economic consequences of this disease for those affected and their families, nearly half of whom face what are considered “catastrophic” costs (>20% of their annual income). In addition, treatment is often delayed, making it impossible to prevent post-tuberculosis sequelae and the impact of this on quality of life. Despite progress and the development of new short-course treatments, the treatment success rate for multidrug-resistant TB is low (68%).
Finally, pending the development of new vaccines, the implementation of preventive treatment, whose effectiveness has been widely demonstrated, is progressing too slowly, with only 21% of family contacts and 56% of PLHIV benefiting from it. Short-course treatments that facilitate adherence are also slow to be implemented.

Sexually transmitted infections (STIs), whether bacterial (such as syphilis, gonorrhea, and chlamydia) or viral (such as papilloma virus and genital herpes), represent a major public health problem worldwide, with nearly 1 million cases per day globally, a quarter of which occur in sub-Saharan Africa. If left untreated, they can lead to serious complications, cervical cancer, reproductive health problems (infertility, ectopic pregnancies, adverse pregnancy outcomes including intrauterine death and prematurity), neonatal infections, and an increased risk of HIV transmission.
Screening and treatment remain inadequate, and the syndromic approach, which exposes both to underdiagnosis of STIs with few symptoms (particularly common in women) and to overprescription, which promotes the emergence of resistance, does not allow for appropriate treatment.
Young people and key populations are particularly at risk due to stigma, lack of appropriate health services, lack of awareness of the importance of these infections, and weak prevention programs.
Priorities for countries in West and Central Africa include integrating activities targeting improved STI diagnosis and treatment into SRHR programs, screening and treatment of syphilis as part of the triple elimination strategy, the development of HPV vaccination, screening and treatment for HPV and cervical cancer, and civil society advocacy for legislation that is more supportive of sexual and reproductive rights and health.

The 10th leading cause of death worldwide
Hepatitis B is a major public health problem. An estimated 254 million people suffer from chronic hepatitis B, resulting in 1.2 million deaths each year from cirrhosis and liver cancer. A quarter of people infected with hepatitis B live in West and Central Africa, where the average prevalence among adults is estimated at between 8% and 12%, one of the highest in the world. While vaccination through expanded immunization programs represents real progress, vaccination coverage is advancing slowly, and too few countries in West and Central Africa are achieving vaccination at birth, which is essential to reduce transmission of this infection to newborns. This intervention is all the more essential given that 90% of hepatitis B-related deaths are the result of infection at birth or in early childhood. Triple elimination programs, which aim to reduce vertical transmission of HIV, syphilis, and hepatitis B, are an opportunity to finally tackle hepatitis B.
However, screening, monitoring, and treatment of people living with hepatitis B and related complications are major challenges. There are many causes, but the lack of trained human resources, the lack of structured health systems, and the lack of funding, as is the case for the response to HIV, TB, and malaria, are the main ones. Screening, testing to determine the stage of the disease and identify treatment options, treatment of hepatitis B and related complications, and follow-up care for people living with hepatitis B are largely unavailable in most countries and patients and their families must cover the costs.

West and Central African countries are particularly vulnerable to emerging infectious diseases, such as Ebola, Lassa fever and, more recently, Mpox, which are exacerbated by deforestation and climate change.
Huge progress has been made in terms of epidemiological surveillance and rapid response capacity following the Ebola epidemic. However, each of these emergencies profoundly destabilizes health systems and jeopardizes prevention, screening, and management activities for all other health issues. Strengthening health systems to increase their resilience to emergencies is a priority.

Today, access to sexual and reproductive health (SRH) and the full expression of rights remain significant challenges. Women, in particular, face considerable difficulties in exercising control over their own bodies. Vulnerable and marginalized groups encounter numerous obstacles in accessing quality care. Despite progress, West Africa is experiencing a slowdown in advancements made so far. The region accounts for a substantial proportion of the continent’s maternal deaths. It is also in West Africa that the experience of motherhood among girls under the age of 15 is most widespread, exposing them to serious complications. Young girls there have a 20% chance of becoming pregnant during adolescence. The region also has the highest rate of unmet need for contraception among adolescent girls.
The implementation of comprehensive sexuality education programs faces strong resistance. Additionally, gender-based violence continues to impact life courses, reflecting deep social inequalities.
In 2023, Solthis produced a report titled ‘For a Feminist Approach to Healthcare: Promoting Sexual and Reproductive Health and Rights for All,’ highlighting our commitment to more inclusive care. Reflecting the strategies deployed by Solthis and its partners in the field, the feminist approach to healthcare that we offer is based on three pillars:
- Empowering women to act and promoting self-care and reappropriation of the body;
- Integrating the fight against gender-based and sexual violence into all actions: prevention, risk reduction and response;
- Focusing services on individuals, particularly women, and taking their specific needs into account.
Solthis’ positioning and actions to promote sexual and reproductive health
To address the SRH needs of populations, particularly the most vulnerable and marginalized (such as people living with HIV, sex workers, or LGBT+ individuals), Solthis implements interventions that strengthen the exercise of their sexual and reproductive rights and improve access to comprehensive, high-quality SRH services.
The organization recognizes the importance of a comprehensive, integrated approach to supporting individuals in their sexual and reproductive health throughout their lives. Each SRH service is part of a set of interconnected components, with a particular focus on the following priorities:
- comprehensive sex education;
- contraception counsel and services;
- prevention and management of STIs/HIV;
- prevention, screening and management of cervical cancer;
- prevention, screening and management of gender-based violence;
- strengthening the management of young people and adolescents and taking into account the specific needs of people in vulnerable situations;
- integration of SRH and HIV services;
- comprehensive abortion care.
and at the primary health care level:
- prevention of mother-to-child transmission of HIV;
- prenatal care;
- emergency obstetric and neonatal care;
- postnatal care;
- referral to appropriate facilities.

In West and Central Africa, the maternal mortality ratio is 724 per 100,000 live births, the highest in the world. The risk of maternal death in giving life, meaning the probability that a 15-year-old girl will die from complications of pregnancy or childbirth during her lifetime, reached 1 in 27 in 2020 in the region, eight times the world average.
Solthis is committed to the Sustainable Development Goals (SDGs) and the ambition to reduce the global maternal mortality ratio to below 70 per 100,000 live births by 2030. Most of these deaths would be preventable if health systems were strengthened as a whole. Solthis works to ensure the availability and quality of maternal, neonatal and child health services.

The West and Central Africa region has the highest infant mortality rate, with 92 deaths per 1,000 live births in 2021. This means one child in the region dies every 17 seconds (WHO, 2021). This rate is far from the United Nations target of 25 deaths per 1,000 live births by 2030. Within this infant mortality rate, neonatal mortality in West and Central Africa accounts for 30.5 deaths per 1,000. Most of these deaths would be preventable if health systems were strengthened overall.
Pneumonia and diarrhea alone account for 29% of these deaths. Vaccination is one of the best ways to protect children from these diseases. However, 1 in 5 children do not have access to these vaccines. Addressing this issue requires efforts at all levels, from the government to the family, in both the public and private sectors.
Solthis’ projects to improve infant care and collaborate with communities and healthcare professionals exemplify our ambition to combine capacity building, technological innovation, and user empowerment.

Worldwide, cervical cancer (CC) is the fourth most common cancer in women, with 660,000 new cases in 2022. Over 94% of the 350,000 deaths from cervical cancer that year occurred in low- and middle-income countries. In West Africa, cervical cancer is the leading cause of cancer-related deaths in women. Almost all cases of cervical cancer (99%) are linked to infection with high-risk human papillomavirus (HPV), a virus commonly transmitted through sexual contact.
HPV is primarily transmitted through sexual activity, and most people become infected shortly after becoming sexually active. Women living with HIV (WLHIV) are more vulnerable to persistent HPV infection than HIV-negative women; they are six times more likely to develop cancer. Our actions are in line with the WHO global strategy:
- A world where cervical cancer is eliminated as a public health problem.
- A threshold of 4 per 100,000 woman-years (incidence rate) for elimination as a public health problem.
- The following 90-70-90 targets to be achieved by 2030 for countries to be on track for elimination of cervical cancer:
* Vaccination: 90% of girls are fully vaccinated before the age of 15.
* Screening: 70% of women are screened using an effective test at the age of 35 and again at the age of 45.
* Treatment: 90% of women identified as having cervical disease receive treatment.

Gender-based violence (GBV) can be defined as ‘any harmful act committed against a person’s will that is based on socially ascribed differences between males and females’.
Teenagers and young people are particularly exposed to GBV, especially sexual violence. This violence can occur within or outside the family. Several studies on sexual violence show that the vast majority of cases are committed by someone known to the victim. Worldwide, 1 in 10 girls under the age of 20 claim to have been a victim of sexual violence. These figures are probably an underestimate. It is estimated that, all ages combined, 1 in 3 women will be a victim of physical or sexual violence during their lifetime. Periods of social instability and psycho-affective vulnerability, such as adolescence, are recognised as periods in which sexual violence is more prevalent. Furthermore, numerous studies in various countries have revealed the significant frequency of sexual violence in schools. Perpetrated by other students or by the teachers themselves, this violence has a major impact on students dropping out of school and on the number of unwanted pregnancies among them.

The effects of climate change have a direct impact on our health. The impacts are already being observed worldwide: the severity or emergence of certain infectious diseases, antimicrobial resistance, but also an increase in chronic illnesses, deteriorating mental health and food insecurity. The burdens associated with these issues underline the importance of adopting approaches and modes of intervention based on multi-disciplinary collaboration linking human, animal and environmental health, and on contextualized and localized projects, supported by communities on a territorial scale, and including monitoring-evaluation and operational research components. Climate change thus calls for new forms of cooperation in health, at international level and within communities, in order to improve the monitoring and documentation of health risks, support mitigation and adaptation strategies and thus better understand and reduce health impacts.

Climate change is one of today’s greatest health threats. It is significantly altering the fundamental determinants of health. All over the world, heat waves are becoming more intense, and floods and natural disasters more frequent.
These upheavals are weakening already vulnerable healthcare systems, accentuating inequalities and jeopardizing food security, access to water and mental health. Stress, anxiety about the future and forced displacement are all realities that now weigh heavily on the shoulders of many communities.
In the face of this emergency, it is essential to think about health and climate together. This means devising health policies capable of adapting to new climatic risks and more resilient health systems, strengthening warning and prevention systems, but also listening to and involving local communities, often on the front line in the face of upheaval.
Integrating climate issues into public health initiatives is no longer an option, it’s a necessity. This calls for concrete, local responses, as well as international cooperation to better anticipate, adapt and protect populations, now and in the future.
Reducing and mitigating the impact of climate change on health also means acting on the causes, by promoting more sustainable and equitable lifestyles and development that respect the ecosystems on which our survival depends. Because by protecting the planet, we are also protecting our health.